by Ivan Bradshaw
Mistakes in medical coding, such as assigning wrong diagnosis or procedure codes or using inappropriate modifiers, can result in claim rejections. These errors typically stem from insufficient documentation or a misunderstanding of coding rules and guidelines.
To prevent medical coding denials, healthcare providers need to implement a comprehensive documentation strategy. This includes:
Through these efforts, healthcare organizations aim to enhance documentation accuracy,
minimize coding denials, and uphold revenue integrity.
AI plays a significant role in minimizing coding related denials. Below are four of the main
ways that AI can virtually eliminate coding denials.

Analyzing historical data to identify recurring patterns and trends associated with medical coding denials is crucial for understanding their root causes. ML (Machine Learning) algorithms automatically detect patterns that may not be obvious to human analysts.

By leveraging ML and deep learning models, AI can capture complex patterns in data and are highly flexible so provider organizations can anticipate potential medical coding denials before they occur. These models can also analyze various data points to identify patterns indicative of a denial, allowing for proactive intervention to address coding issues before claims are submitted.

Automating the generation of appeal letters and supporting documentation based on denial reasons and relevant clinical data streamlines the appeals process and improves efficiency. When combined with RPA (Robotic Process Automation) AI for claim denials can manage repetitive tasks involved in appeal generation, freeing up human resources for more complex tasks.

Ensuring coding consistency with current guidelines and regulations is essential for reducing the risk of medical coding denials due to non-compliance. ML-based models can analyze coding practices against established guidelines, flagging any discrepancies for review and correction.
Step 1
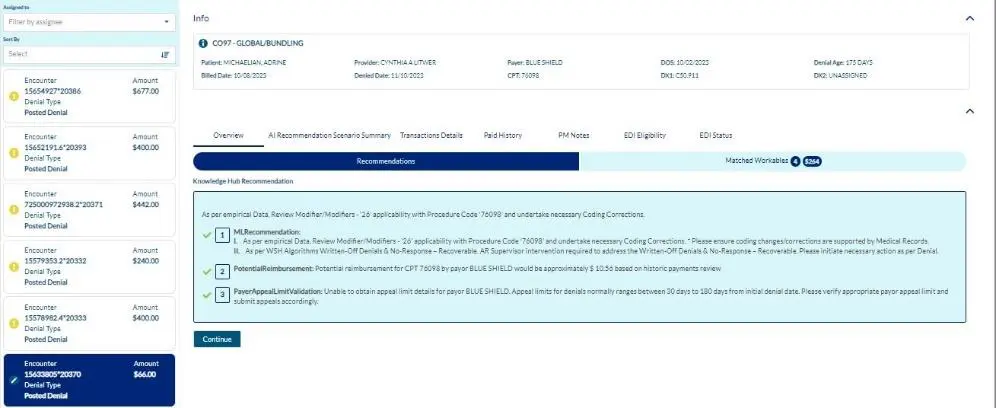
Identify all claims with coding-related denials. By grouping claims with the same or similar reasons, the platform creates leverage and expedites the appeals process.
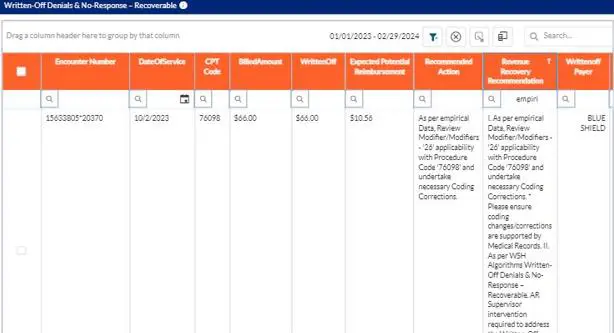
Step 2
The RevEnhance® solution interprets historical data using AI algorithms toprovide guided recommendations. Even the newest staff members can read these recommendations and take the actions that will drive the claims to resolution.
The WhiteSpace Health Revenue Cycle Analytics was purpose-built for the revenue cycle. Our revenue cycle denials management and health information management experts created the platform we needed when managing our own departments. Everything is readily available at go-live so you can immediately unlock the tremendous value in your data to create a predictable and highly efficient revenue cycle.
About Ivan Bradshaw

Ivan Bradshaw is the vice president of product management at WhiteSpace Health. As a revenue cycle management executive with over 20 years of experience, Ivan is adept at building high-performance teams and creating RCM solutions that stop revenue leakage, improve
operational efficiency, and grow top-line performance.
Ivan.Bradshaw@whitespacehealth.com

2424 North Federal Highway, Suite 205
Boca Raton, FL 33431