by Ivan Bradshaw
Authorization refers to the payer’s agreement to pay for specified treatments before the patient receives care. This process is also referred to as preauthorization or prior authorization. As the name suggests, the insurance provider wants to ensure care is necessary before authorizing the planned treatment or service. Failure to obtain insurance approval to render care almost always leads to an authorization denial.
Procedures for obtaining a prior authorization are quite varied in healthcare. In the first step in determining whether an individual patient or service is eligible for coverage, it is necessary to establish whether the planned services require prior authorization or not. The request will be made based on the patient’s health insurance coverage. Before granting coverage, insurance companies must approve requests for necessary medical treatments and benefit conditions.
Preauthorization is a component of medical billing that guarantees claims are processed efficiently and error-free. It is important to note that the preauthorization number and details must be included on the final claim form submitted following the treatment. If there is no pre-approval, invoices are not paid
To prevent authorization denial, providers need to ensure all relevant Information is thoroughly documented, by submitting the authorization requests promptly. Providers need to familiarize themselves with specific authorization requirements and policies of different payers to ensure compliance with their criteria for coverage.
They also need to able proactive in the appeal process by providing additional information or supporting documentation to overturn the decision as appropriate. AI plays an important role in reducing.

By using AI based predictive models or rule-based systems can encode
domain-specific knowledge and business rules governing authorization
decisions and anomaly detection techniques can identify unusual patterns or
outliers in authorization data that may indicate potential denial risks. Algorithms
can be used for this purpose to analyze historical authorization data to predict
which requests are likely to be denied. By identifying patterns and trends, AI can
help healthcare providers adjust their approach to authorization requests,
increasing the likelihood of approval.
The WhiteSpace Health Platform uses ML models as support tools for claim
resolution by identifying claims denied for prior authorization that are still
collectible.

Based on patterns in the data, the platform identifies claims with successful
resolutions, and it suggests the most appropriate actions to increase the
likelihood of successful resolution.
When staff follow these guided steps, they optimize the efficiency of the
revenue cycle and lower denial resolution expenses.
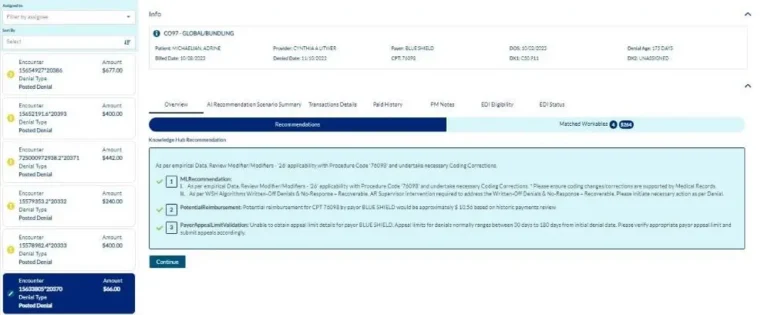
While there are a number of actions that healthcare organizations can take to minimize prior authorization denials, unfortunately some will still occur. When they do, AI and ML in the WhiteSpace Health Platform stand ready to identify the affected claims that can still be paid and deliver guided steps to resolve them, giving your organization the best chance to
get paid – quickly
About Ivan Bradshaw

Ivan Bradshaw is the vice president of product
management at WhiteSpace Health. As a revenue
cycle management executive with over 20 years of
experience, Ivan is adept at building high-performance
teams and creating RCM solutions that stop revenue
leakage, improve operational efficiency, and grow top
line performance.
Ivan.Bradshaw@whitespacehealth.com

2424 North Federal Highway, Suite 205
Boca Raton, FL 33431